Carbamazepine, typically used in epilepsy and bipolar disorder treatments, demonstrated efficacy in reducing pain and minimizing cartilage loss in mouse models.
An epilepsy drug called carbamazepine may revolutionise the way osteoarthritis is treated, according to a ground-breaking study that was published in Nature. The study, led by Dr. Chuan-Ju Liu from Yale University School of Medicine, explored the role of a specific sodium channel, Nav1.7, in neurons and cartilage cells, revealing its crucial connection to osteoarthritis progression.
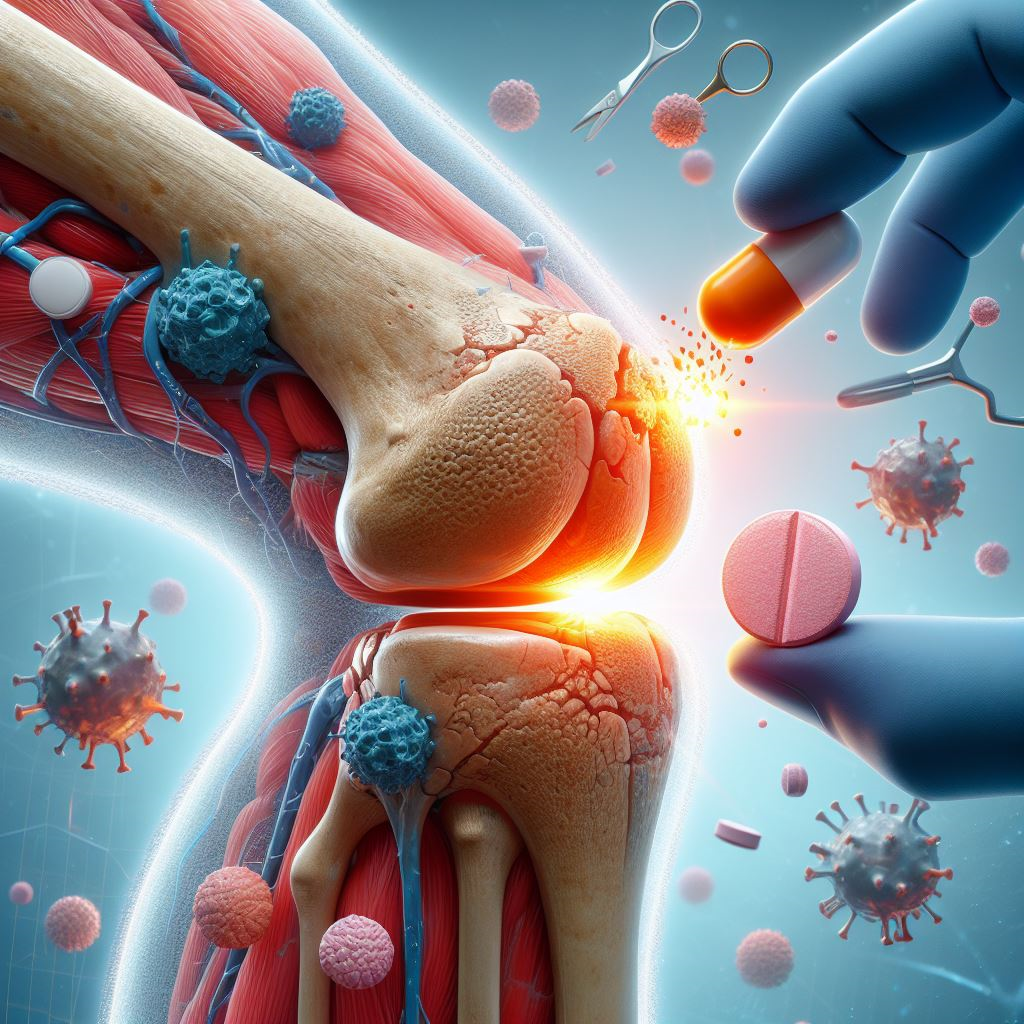
Osteoarthritis, a chronic and painful condition affecting joints, has long posed challenges for effective management. Current treatments primarily focus on alleviating pain rather than addressing the underlying cartilage breakdown. However, this recent research provides a glimmer of hope for a more comprehensive approach.
The study delves into the intricate cellular mechanisms involved in osteoarthritis, honing in on chondrocytes — the cartilage cells responsible for maintaining joint health — and their interaction with voltage-gated sodium channels, specifically Nav1.7. Through meticulous analysis of mouse models and human cell samples, researchers found elevated levels of Nav1.7 in chondrocytes of individuals with osteoarthritis.
Deleting Nav1.7 in mouse models showed promising results. In neurons, its absence contributed to a reduction in pain, while in chondrocyte cells, it led to significantly less structural damage and slower progression of osteoarthritis. The breakthrough came when the researchers explored the impact of Carbamazepine, an epilepsy medication known for inhibiting Nav1.7 channels.
Study author Dr. Chuan-Ju Liu highlighted the significant findings: “Our discovery of the sodium channel Nav1.7 as a target for both pain relief and disease modification represents a significant stride towards a novel therapeutic strategy to slow down or prevent osteoarthritis progression while concurrently alleviating associated pain.”
Carbamazepine drug, typically used in epilepsy and bipolar disorder treatments, demonstrated efficacy in reducing pain and minimizing cartilage loss in mouse models. While these results are promising, it’s crucial to note that the study’s limitations, derived from mouse models and a limited number of human cell samples, call for cautious optimism.
Dr. Liu emphasized the need for further research before translating these findings into human applications: “There is still a long way to go in translating current findings from animal models to human applications. We need to understand why a low number of sodium channels has such significant effects on chondrocyte biology.”
Despite the preliminary nature of the research, the potential implications for osteoarthritis patients are significant. Dr. Steve Yoon, director of The Regenerative Sports and Joint Clinic at Cedars-Sinai Kerlan-Jobe Institute, stressed the importance of a multidisciplinary approach in managing osteoarthritis.
He noted, “Common treatments for osteoarthritis require a multidisciplinary approach,” including modalities such as ice and heat, topical creams with anti-inflammatory medications, and oral medications like acetaminophen and ibuprofen.
The next steps involve exploring new therapeutic strategies centered on blocking Nav1.7 channels and investigating gene therapy approaches to reduce the production of these channels. The ultimate goal is to bridge the gap between animal models and human treatments, offering a more manageable future for osteoarthritis patients.
As the study raises hopes for a breakthrough in osteoarthritis treatment, individuals grappling with the condition may find solace in the prospect of a more targeted and effective approach. While Carbamazepine’s potential in osteoarthritis treatment holds promise, the journey from mouse models to human trials is a critical phase that will determine the drug’s viability as a revolutionary solution for this widespread and debilitating condition.