The incidence and geographic range of numerous vector-borne diseases, such as Lyme borreliosis and canine leishmaniasis, are rising globally.

Many arthropods, including insects, can be a nuisance to people and pets. They can infect you with dangerous germs unseen to the naked eye but can quietly kill you, such as viruses, bacteria, protozoa, and helminths, in addition to simply “bugging” you.
Many members of the phylum Arthropoda, including ticks (order Ixodida), mosquitoes (family Culicidae), sand flies (subfamily Phlebotominae), kissing bugs (subfamily Triatominae), fleas (order Siphonaptera), and lice (order Phthiraptera), are effective carriers of significant pathogenic organisms for both animals and humans.
Malaria, leishmaniasis, and Chagas disease have a significant worldwide impact and are disproportionately prevalent in underdeveloped nations in tropical and subtropical areas. For example, 3.3 billion individuals in 97 countries and territories are thought to be at risk of malaria.
Similar estimates for cutaneous and visceral leishmaniasis cases per year in 98 nations and three territories range from 0.2 to 0.4 and 0.7 to 1.2 million, respectively.
Finally, there is an underappreciated burden of neglected infections (not just vectorborne) of poverty in developed countries, such as the United States and European nations. These infections include ascariasis, trichuriasis, toxocariasis, trichinellosis, opisthorchiasis, taeniasis, echinococcosis, leishmaniasis, and Chagas disease.
Many human-affecting vector-borne diseases have zoonotic origins. Wildlife, cattle, and companion animals are reservoir hosts for several diseases. For instance, some infections that can infect people and cause diseases, such as Dirofilaria immitis, Leishmania infantum, and Rickettsia conorii, may be carried by dogs.
Even though the role of canines as reservoirs for some of these pathogens is not fully understood, controlling canine vector-borne diseases is desired under the One Health ethos and may eventually lower the risk of pathogen exposure in humans.
The One Health Initiative highlights the importance of veterinary and human medical cooperation to protect the health and wellness of people, animals, and the environment.
Spread of Vector-Borne Diseases
The incidence and geographic range of numerous vector-borne diseases, such as Lyme borreliosis and canine leishmaniasis, are rising globally. Several new infections transmitted by ticks and mosquitoes have also been identified in recent years.
Examples of ailments that have (re-)emerged in various parts of the world include Lyme borreliosis, tick-borne encephalitis, Crimean-Congo hemorrhagic fever, dengue fever, West Nile fever, Chikungunya fever, plague, bartonellosis, and other tick-borne rickettsioses.
The growing knowledge of researchers, doctors, veterinarians, and other healthcare professionals has contributed to recent discoveries and the popularization of molecular biology tools (such as DNA sequencing and PCR).
Over the past few decades, rickettsial pathogens have frequently been found in both canines and people. Among these are Anaplasma phagocytophilum, Anaplasma platys, Rickettsia rickettsii, Rickettsia conorii, Rickettsia massiliae, Panola Mountain Ehrlichia, Candidatus Neoehrlichia mikurensis, and several additional spotted-fever Rickettsiae.
In several cases, these microorganisms were initially found in ticks before being positively identified as human pathogens. It implies that some Rickettsiae that have lately been isolated from ticks and other animals but whose pathogenicity is unknown may later turn out to be human pathogens.
Regarding this, various clinical and laboratory data, including serological testing, immunohistochemistry labelling, cell culture isolation, and molecular approaches, should be used to determine whether a certain rickettsial organism is a cause of disease in people.
The nematode Onchocerca lupi is a typical illustration of a developing infection connected to dogs and humans. O. lupi, first identified in wolves in 1967, is now widely accepted as the root of ocular disease in humans and canines in the USA, numerous European nations, North Africa, the Middle East, and North Africa. Although O. lupi DNA has recently been found in black flies (family Simuliidae) in the USA, the biological vector of the parasite is still unknown.
Rangelia vitalii is another example of a developing vector-borne pathogen identified in dogs but has not yet been reported in humans. The canine rangeliosis protozoan, spread by the yellow dog tick Amblyomma aureolatum, is a serious condition.
Canine rangeliosis, first identified in Brazil in 1910, was a mysterious and little-known condition for many years, but it is now known to exist in Uruguay and Argentina, among other nations in South America.
Clinically, the condition is like other canine vector-borne illnesses, like babesiosis and ehrlichiosis, which could make a diagnosis more difficult in regions where these illnesses are sympatric. Climate change, deforestation of tropical forests, land-use change, urbanization, population growth and migration, habitat fragmentation, animal movements, and biodiversity loss may influence the introduction of vector-borne diseases.
Veterinarians’ and doctors’ increased focus on, and awareness of vector-borne diseases may potentially contribute to discovering these illnesses in new geographical areas. For instance, recent research has shown definite shifts in the geographic distribution of significant tick vectors, including the castor bean tick Ixodes ricinus and the spirochete Borrelia burgdorferi, which is the cause of Lyme borreliosis.
Climate change and, to a lesser extent, host population changes have been connected to changes in I. ricinus distribution. The southbound and northward migration of canine leishmaniasis and dirofilariasis in Italy are further recent instances of shifting distribution patterns and rising incidence of canine vector-borne diseases.
The expansion of phlebotomine vectors into northern regions due to climatic change and the introduction and dissemination of Aedes albopictus throughout the 1990s across several Italian regions may also have contributed to these developments, in addition to veterinarians’ improved awareness.
Additionally, this process may have been influenced by the movement of diseased canines from endemic to nonendemic areas. The current and shifting distribution of vector-borne infections directly impacts physicians’ and veterinarians’ daily activities.
The introduction and establishment of pathogens into new areas may impact their clinical practice, not only because they may not be equipped to diagnose novel diseases but also because co-infections may obscure the clinical picture and postpone the final diagnosis, ultimately raising the possibility of life-threatening complications.
Indeed, co-infections in humans and animals are becoming more widely recognized and may alter how a disease develops. Updated maps and ongoing training for health organizations, nurses, doctors, and veterinarians are essential to raising knowledge of emerging vector-borne diseases in various areas.
The Most Extreme Disease Vectors: Mosquitoes or Ticks?
A variety of arthropod species can potentially transmit diseases to humans and dogs. There are other less well-known vectors, such as the stable fly Stomoxys calcitrans, as well as insects, including mosquitoes, sand flies, black flies, biting midges (family Ceratopogonidae), fleas, kissing bugs, and bedbugs (family Cimicidae) (family Muscidae).
As in the case of the fruit fly Phortica variegata (subfamily Steganinae), which may spread infectious third-stage larvae of the eyeworm Thelazia callipaeda while feeding on lachrymal secretions of animals, including dogs and humans, other flying insects that feed on sources other than blood may also act as vectors.
Ticks, fleas, lice, and several types of mites are non-flying arthropods that can spread infections of significant medical and veterinary significance.
Arthropods that feed on blood have exceptional blood-swallowing capacities, which can lead to anemia and other hematological problems in their hosts. Mosquitoes came in at number six on the list of the Top 10 most extreme bloodsuckers on Earth, kissing bugs came in at number four, bedbugs at number three, fleas at number two, and ticks at number one. Some ticks can consume blood about 200–600 times their body weight.
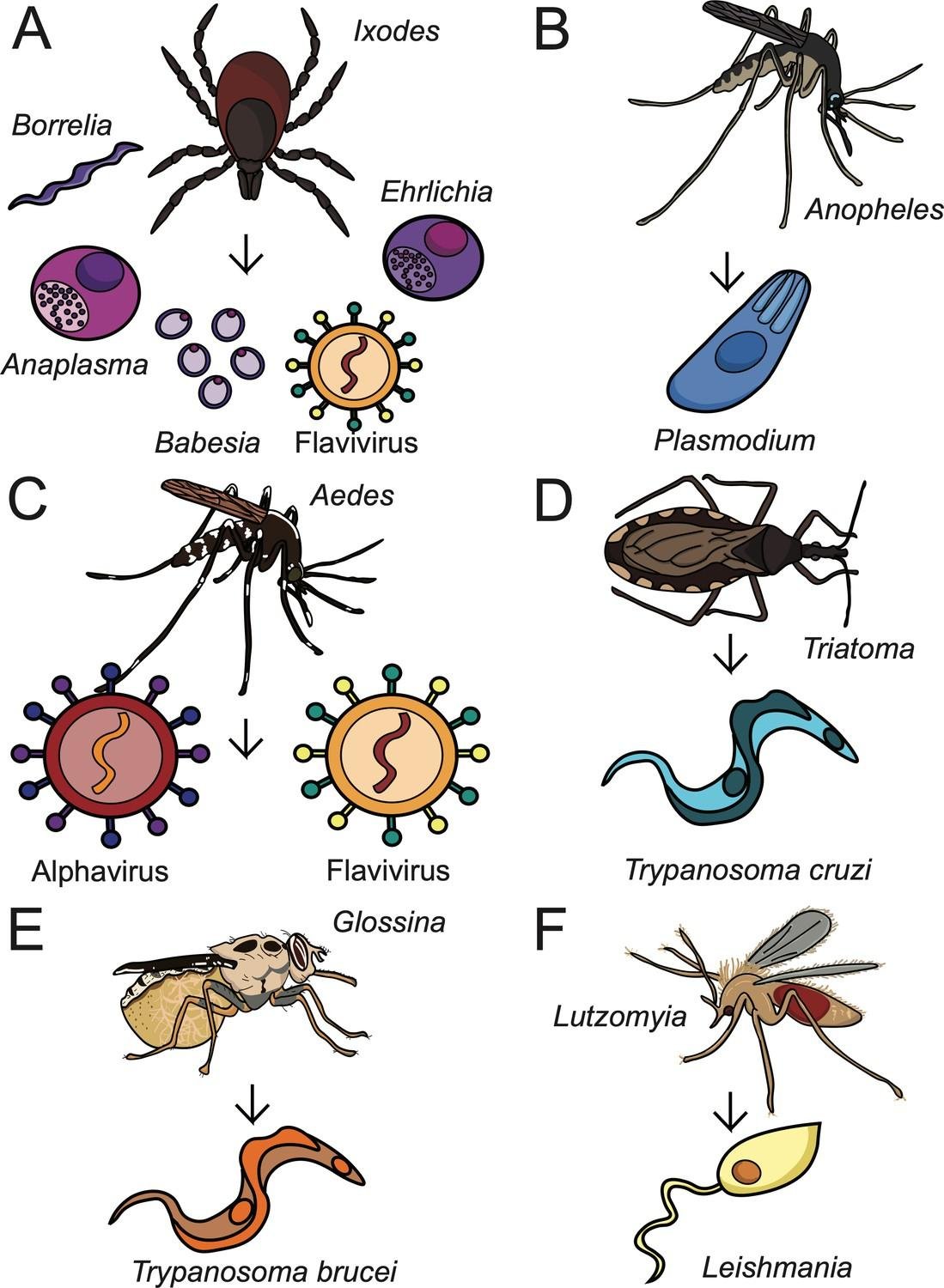
Figure: Depicting the role of various vetors in diseases transmission A. ticks, B. Mosquito (Anopheles), C. Mosquito (Aedes), D. Bug (Triatoma), E. Testse Fly (Glossinidae), F. Fly (Lutzomiya).
The most significant carriers of infections for both humans and animals, according to the literature, are typically either ticks or mosquitoes. For instance, ticks have the potential to spread a wide range of infections to humans and canines.
However, mosquitoes may be regarded as the most extreme disease vectors in terms of global morbidity and mortality in humans because they are the main carriers of parasites that cause malaria and filariasis as well as significant arboviruses like dengue fever, Chikungunya, yellow fever, West Nile fever, Japanese encephalitis, and others.
An estimated 584,000 individuals died from malaria in 2013 (estimated 367 000–755 000), 90% of which occurred in Africa and largely affected children under five years. In light of this, controlling disease vectors is crucial from a veterinary and public health standpoint. To create better control tactics, it will also be vital to have a deeper grasp of their biology and ecology.
Vector Control: New Knowledge, New Strategies
Even if it may not be simple to raise some of these vectors in the laboratory, our understanding of the biology and ecology of disease vectors has greatly expanded over the past few decades. Any hematophagous arthropod’s blood-feeding behavior has been thoroughly investigated because it is a crucial stage in their life cycle.
To produce eggs, females need blood as a supply of nutrients. Additionally, most vector-borne diseases are spread through blood feeding; the exceptions are Hepatozoon protozoa, which are spread when dogs consume an infected vector, and Thelazia callipaeda nematodes, which are spread by secretophagous flies and Hepatozoon protozoa, respectively.
These details must be emphasized to dog owners if you want any control program to be successful. As a result, research into feeding techniques (such as host-finding strategies and host preferences) and transmission timeframes have taken precedence on the agenda of those studying vector-borne diseases.
In field-collected vectors, new techniques have been created for pathogen detection and blood-meal identification. For various diseases, fresh information on transmission times has been acquired. One recent study, for instance, found that ticks had to be connected to the host for at least three hours to transmit E. canis.
According to a different study, fed ticks can transmit R. rickettsii after only 10 minutes of attachment, whereas unfed ticks must remain attached to the host for at least 10 hours. These studies emphasize the significance of eliminating, discouraging, and killing blood-seeking vectors as quickly as possible to prevent prolonged attachment, which may raise the risk of disease transmission.
It is crucial for L. infantum, transmitted through bites from female sand flies infected within minutes of feeding. In fact, this idea has encouraged pharmaceutical companies to invest in research and development (R&D) to provide long-lasting medications with deterrent and quick-killing capabilities.
The knowledge gathered over the last few decades has also paved the path for fresh research to create new control measures, like antivector vaccinations, biological control agents, and genetically modified insects.
However, little progress has been achieved in creating new, efficient tactics, such as anti-tick vaccinations, to reduce ticks and diseases. Like mosquito control, genetic engineering and biological agents have been used in some nations, but they haven’t always been effective in bringing down mosquito populations and, more importantly, the prevalence of diseases like dengue fever.
Integrated vector control programs frequently include chemical control and various non-chemical techniques. Chemical management can often be the most crucial and, ultimately, the sole method for managing various vectors and avoiding the transmission of diseases that they spread.
Kashif Hussain, Maria Kausar, Muhammad Sohail Sajid and Urfa Bin Tahir from Department of Parasitology, University of Agriculture, Faisalabad-Pakistan