Johns Hopkins engineers and cancer researchers developed deep-learning technology to predict cancer-related protein fragments that can possibly activate immune system reactions.
Johns Hopkins engineers and cancer researchers developed deep-learning technology to predict cancer-related protein fragments that can possibly activate immune system reactions. This strategy might be used to generate personalized immunotherapies and vaccines, overcoming challenges in clinical testing.
Johns Hopkins Kimmel Cancer Center, Johns Hopkins Institute for Computational Medicine, and Bloomberg Kimmel Institute for Cancer Immunotherapy conducted a study to show that the BigMHC deep-learning method can recognize protein fragments on cancer cells that cause an immune response that kills tumor cells. This is essential for figuring out how immunotherapy works and creating individualized cancer treatments.
Activating a patient’s immune system to eliminate cancer cells is the goal of cancer immunotherapy, according to Rachel Karchin, Ph.D., professor of biomedical engineering, oncology, and computer science and a key figure in the Institute for Computational Medicine.
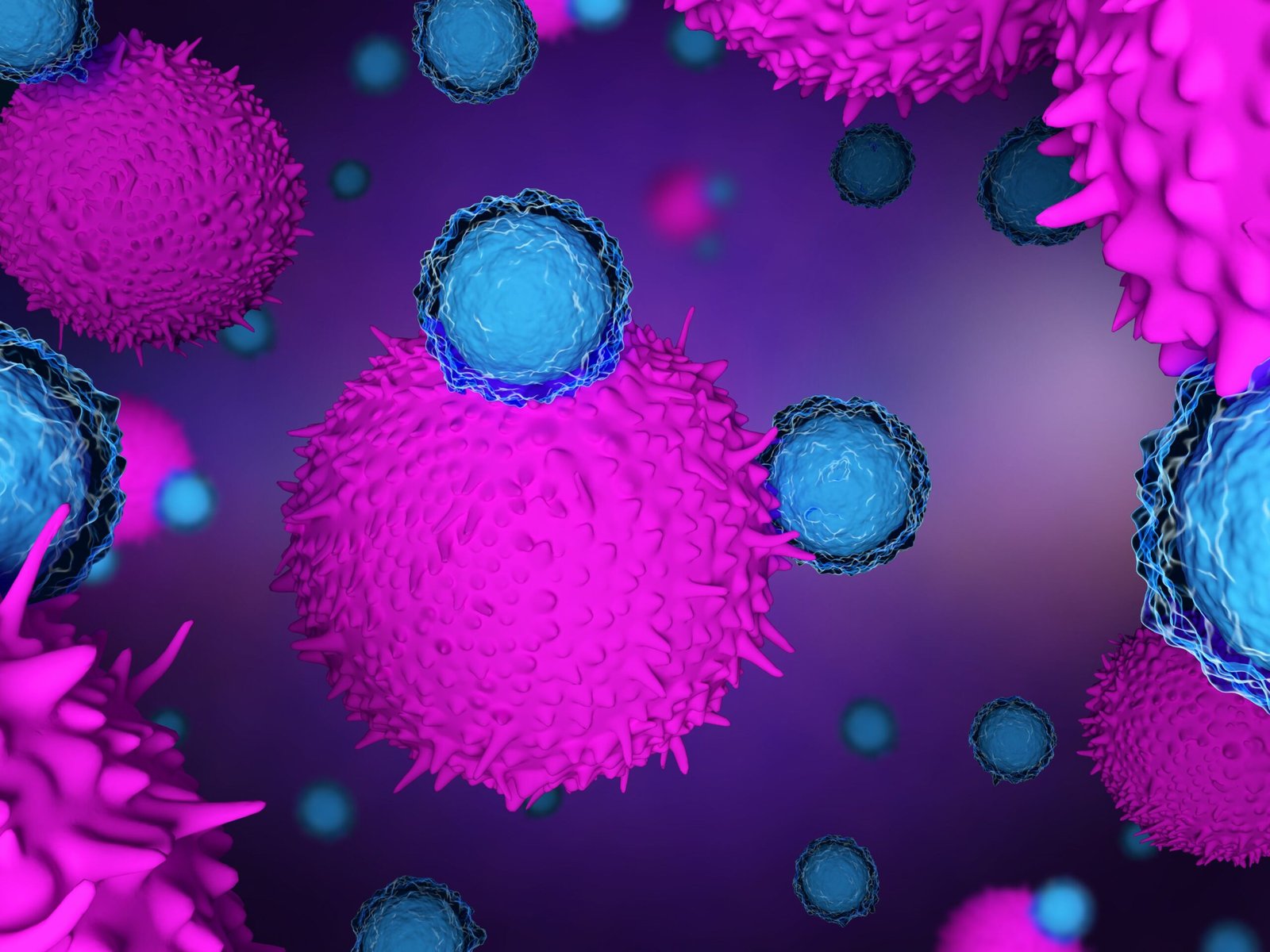
T cell attachment to cancer-specific protein fragments on the cell surface is a crucial stage in the process of the immune system recognizing cancer cells.
Mutation-associated neoantigens, which are cancer protein fragments that trigger an immune response that kills tumors, may result from genetic alterations (or mutations) in cancer cells.
Tumors have unique neoantigens that determine their foreignness. Scientists can identify mutation-associated neoantigens by analyzing the cancer’s genome. This could enable personalized cancer vaccines or immune therapies, and inform patient selection. However, current methods are time-consuming and costly, relying on labor-intensive, wet laboratory experiments.
Transfer learning was used to train BigMHC, a collection of deep neural networks, to handle resource-intensive neoantigen validation. They honed it for T-cell recognition, a later stage with less data, after learning to recognize antigens on the cell surface, an early step of the adaptive immune response. This method made use of a wealth of data to develop a model of antigen presentation, which was then improved to forecast immunogenic antigens.
BigMHC was proven to be more accurate in predicting antigen presentation than competing approaches by the researchers after being evaluated on a sizable independent data set.
They then evaluated BigMHC using data from associate professor of oncology and research co-author Kellie Smith, Ph.D., of the Bloomberg-Kimmel Institute for Cancer Immunotherapy, and discovered that BigMHC considerably outperformed seven other approaches in identifying neoantigens that cause T-cell response. According to Karchin, “BigMHC has outstanding accuracy at predicting immunogenic neoantigens.”
“There is an urgent, unmet clinical need to tailor cancer immunotherapy to the subset of patients most likely to benefit, and BigMHC can shed light into cancer features that drive tumor foreignness, thus triggering an effective anti-tumor immune response,” says study co-author Valsamo “Elsa” Anagnostou, M.D., Ph.D., director of the thoracic oncology biorepository, leader of the Johns Hopkins Molecular Tumor Board and Precision Oncology Analytics, and associate professor of oncology in the Kimmel Cancer Center.
The team is testing BigMHC in immunotherapy clinical trials to determine its potential in filtering through hundreds of thousands of neoantigens to trigger an immune response.
The goal is to guide cancer immunologists in developing personalized vaccines or immunotherapies for multiple patients, according to lead author Benjamin Alexander Albert. Albert, a Ph.D. student at the University of California, San Diego, was an undergraduate student researcher at The Johns Hopkins University when the study was conducted.
BigMHC and similar machine-learning-based technologies, in the opinion of Karchin and her colleagues, can aid cancer researchers and doctors in sorting through the enormous volumes of data necessary to create more individualized approaches to cancer therapy. According to Karchin, “Deep learning has a significant role to play in clinical cancer research and practice.”