Salmonella contains more than 2500 serovars of S. enterica, based on a system devised by Kaufmann and White in which somatic (O) and flagellar (H) antigens are identified.
Salmonella species are usually motile, gram-negative, anaerobe, bacilli-shaped, flagellated, and facultative intracellular of worldwide importance, causing as many as 1.3 billion cases of disease annually associated with human as well as animal infections, and they do not ferment lactose.
Rarely, lactose-fermenting strains are encountered. Some indications show that 15,000 to 150,000 years ago, a common S. typhi ancestor existed when humans were still hunters and spreading across the planet.
Salmonella spp. infections lead to high morbidity rates in both developing and industrialised countries and high mortality, mainly in the poorest nations with poor hygienic conditions in the developing world.
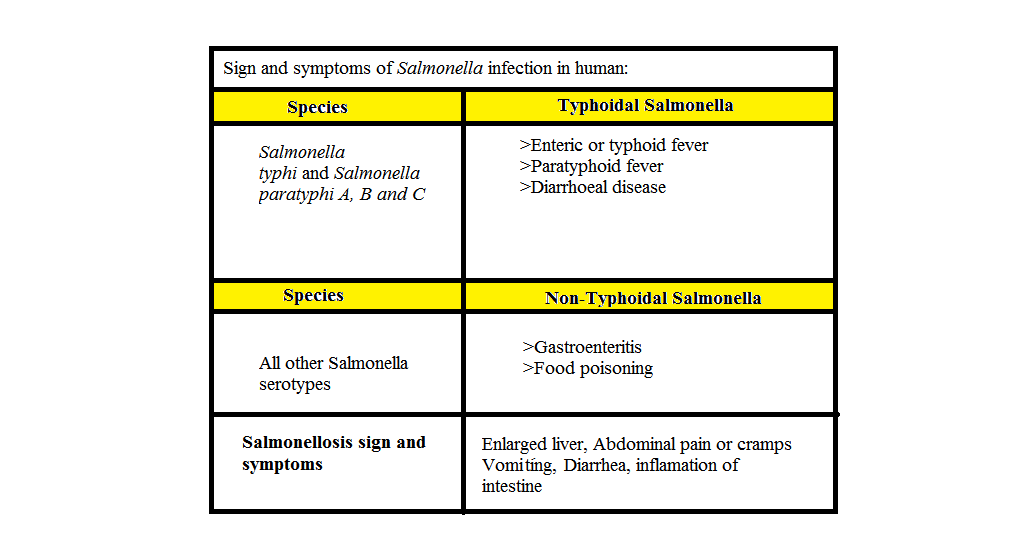
Clinical syndromes caused by Salmonella infection in humans are divided into typhoid fever, caused by Salmonella typhi and Salmonella paratyphi, and a range of clinical syndromes, including diarrheal disease, caused by a large number of non-typhoidal Salmonella serovars (NTS).
Salmonella contains more than 2500 serovars of S. enterica, based on a system devised by Kaufmann and White in which somatic (O) and flagellar (H) antigens are identified. Occasionally, capsular (Vi) antigens may be detected that have been identified as belonging to six subspecies as follows: enterica, salamae, arizonae, diarizonae, houtenae, and indica, while S. bongori has no subspecies.
Subspecies are further subdivided into serovars that are differentiated by their flagellar, carbohydrate, and lipopolysaccharide (LPS) structures, according to the Centres for Disease Control (CDC). Salmonella serotypes occur worldwide.
They infect many mammals, birds, and reptiles and are excreted mainly in feces. Ingestion is the main route of infection in salmonellosis, although it can also occur through the mucosae of the upper respiratory tract and conjunctiva.
Organisms may be present in water, soil, animal feeds, raw meat, and vegetable material. The source of environmental contamination is invariably feces. The former species are the causative agents of enteric fever, and they include S. enterica, subspecies enterica, and serotypes Typhi and Paratyphi (Salmonella typhi and Salmonella paratyphi).
Both focal and invasive presentations of NTS are associated with high mortality. The commonest cause of invasive NTS disease worldwide is advanced HIV disease, which is associated most strikingly with recurrent bacteremia. These associations with immune suppression and poor outcomes are not seen in typhoid fever.
Route of Transmission in Humans:
- Ingestion is the main route to Salmonella infection.
- Direct contact with animals.
- Contaminated food and water.
- Person-to-person transmission
Organisms are also present in:
- Water
- Soil
- Animal feeds
- Raw meat
- Vegetable material
- Faeces.
Pathogenesis:
- The pathogenesis of Salmonella is a phenomenon that varies depending on dose quantity, age, immune status of the host, and different serovars.
- The infection is caused by the ingestion of bacteria through contamination of food or water.
- The serotypes of Salmonella enterica infect different host animals in a wide range of ways. According to some case studies, host-adapted serotypes tend to cause more severe disease than non-adapted serotypes. In farms, disease is sometimes endemic, with a high incidence in clinics, but the occurrence of clinical infection is low.
- The virulence of Salmonella serotypes relates to their ability to invade cells, replicate in epithelial cells (intracellularly), have a complete lipopolysaccharide coat, and elaborate on at least three toxins: 1. Endotoxins: They produce fever when released into the bloodstream of the infected person. 2. Enterotoxin: They may not be involved in causing diarrhoea in Salmonella infection, which is caused by food poisoning, but reduces a secretary response of epithelial cells. 3. Cytotoxin: They contribute to iron-chelating structural damage to intestinal epithelial cells as a result of inhibiting protein synthesis, and iron-chelating proteins provide iron from the iron-binding proteins, which is necessary for bacterial growth.
- Several other virulence factors contribute to the establishment of disease, like adhesion pili, surface polysaccharide O antigen, flagellar H antigen, and fimbriae production of colicin and porins, as well as the ability to resist the lethal effects of large plasmids, whose size is 30–60 megadaltons. Systemic disease is caused by the survival of bacteria within macrophages. Salmonella pathogenicity islands (SPI) and virulence plasmids are playing a very important role in the virulence of salmonellae.
- In some human and animal cases, salmonella causes stress due to overcrowding, transportation, surgery, pregnancy, oral antimicrobial therapy, and chronic diseases. Salmonellae have the ability to survive in gastric acid, repair the damage that is caused by acid stress, and easily pass the gastric acid barrier.
- The acid tolerance ability of salmonella protects them from inorganic and organic acid stress through the production of acid shock proteins. Food matrix is also protecting salmonella in the stomach; if foods contain high fat, the infectious dose rate is low.
- The adherence of salmonella to the mucosa occurs through fimbrial attachment in the intestine.
- After the attachment of organisms, they induce ruffling of the cell membrane. This ruffling is part of the mechanism whereby the organisms are taken up into non-phagocytic cells.
- Type III secretion system (TTSS) is one of the major effects of pathogenicity-island, which is found in all serotypes of S. entrica. This Type III secretion system transfers the virulence factors of bacteria by forming a needle-like structure. The Type III secretion system (TTSS) is a complex of proteins that activate secretory pathways and alter ion balance within the cell.
- Effector proteins are produced as a result of neutrophil recruitment and inflammation, together with the alteration of fluid and ion balance, which causes diarrhoea.
- Effector proteins are also involved in the formation of Salmonella-induced filaments. The function of these Salmonella-induced filaments is unknown, but they play a role in intracellular replication and protect intracellular organisms from bactericidal compounds produced by the host cell, such as reactive oxygen intermediates.
- Some virulence genes play a role in intracellular survival and are involved in invasion.
Clinical Signs and Symptoms Caused by Salmonella Infection in Humans:
The clinical outcome of salmonella infection is based on typhoidal salmonella, non-typhoidal salmonella infection, and salmonellosis, which cause enteric fever, typhoid fever, paratyphoid fever, gastroenteritis, food poisoning, abdominal pain, vomiting, and diarrhea. These symptoms are classified in Table 1.
Epidemiology:
Salmonella infection is spread all over the world. In both developing and developed countries, Salmonella highly affects children and adults aged 5–20.
In salmonella infection, epidemiology depends on the serotype of Salmonella involved in the infection. For example, S. typhi and S. paratyphi cause chronic or severe disease (typhoid fever) in humans but do not cause it in non-human hosts.
Typhoid disease is highly reported in medically underserved communities. On the other hand, non-typhoidal salmonella infection involves self-recovery, which affects communities all over the world.
Prevention Measures for Salmonella Infection:
- Cooked food properly
- Safe food handling practices
- Sanitation measures
- Vaccination
- Proper hand washing after contact with animals and meat products
- Safe water access
This article is jointly authored by Muhammad Hamza, Aziz ur Rehman, Waqas Haider, Qosain Ahmad, and Usman Ali from the University of Veterinary and Animal Sciences Lahore, subcampus Jhang.