Anthrax is a severe disease that affects virtually all mammalian species, including humans. The disease occurs worldwide and is endemic in some countries and defined regions of other countries.
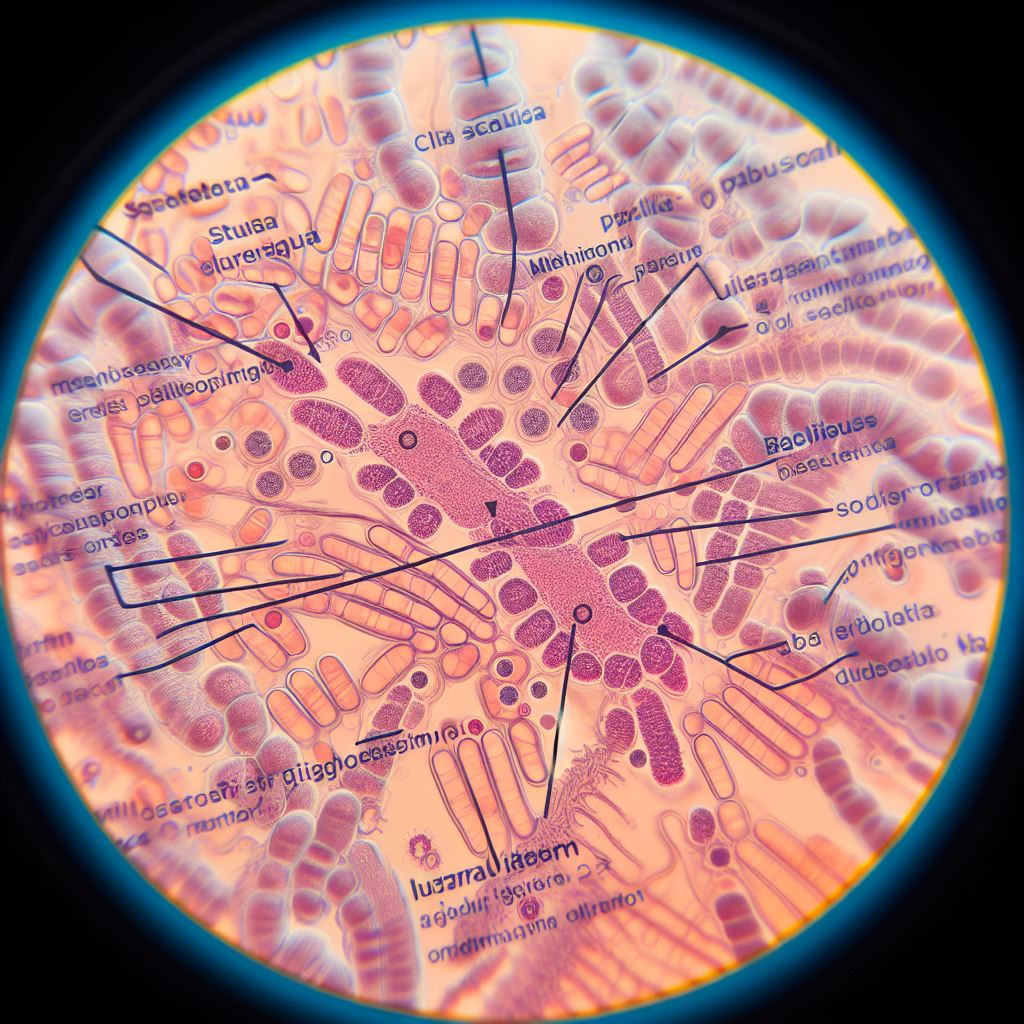
Most Bacillus species are large, Gram-positive, endospore-producing rods up to 10.0 μm in length. A few non-pathogenic species are Gram-negative, and organisms in smears prepared from old cultures decolorize readily. Anthrax is a severe disease that affects virtually all mammalian species, including humans. The disease occurs worldwide and is endemic in some countries and defined regions of other countries.
Ruminants are highly susceptible, often developing a rapidly fatal septicaemic form of the disease. Pigs and horses are moderately susceptible to infection, while carnivores are comparatively resistant. Birds are almost resistant to infection, a characteristic attributed to their relatively high body temperatures. In smears from tissues or cultures, cells occur singly, in pairs, or in long chains.
The genus is comprised of more than 200 species with diverse characteristics. Bacillus species are catalase-positive, aerobic, or facultatively anaerobic, and most species are motile, although the major pathogen, Bacillus anthracis, is non-motile.
Most species are saprophytes with no pathogenic potential. However, they often contaminate clinical specimens and laboratory media. Bacillus anthracis is the most important pathogen in the group. The name Clostridium piliforme has been proposed for Bacillus piliformis, the agent of Tyzzer’s disease. Bacillus larvae, a major pathogen of bees, has been reclassified as Paenibacillus larvae subsp. Larvae.
Usual Habitat:
Bacillus species are widely distributed in the environment, mainly because they produce highly resistant endospores. In soil, endospores of B. anthracis can survive for more than 50 years. Some Bacillus species can tolerate extremely adverse conditions such as desiccation, high temperatures, and chemical disinfectants.
Pathogenesis and Pathogenicity:
The virulence of B. anthracis derives from the presence of a capsule and the ability to produce a complex toxin. Both virulence factors are encoded by plasmids.
and are required for disease production. The plasmid PXO1 encodes the three components that form two exotoxins; the genes that regulate their expression are also found on the plasmid. The genes encoding capsule production and their regulators are found on plasmid PXO2. The expression of virulence factors is regulated by a number of variables, including host temperature and carbon dioxide concentration.
The capsule, composed of poly-γ-D-glutamic acid, inhibits phagocytosis. The complex toxin consists of three antigenic components: protective antigen, oedema factor, and lethal factor. Individually, each factor lacks toxic activity in experimental animals, although protective antigens induce antibodies, which confer partial immunity. Protective antigen acts as the binding moiety for both the oedema factor and the lethal factor.
Oedema factor is a calmodulin-dependent adenylate cyclase, and once it has entered cells following binding to protective antigens, it causes increased levels of cyclic AMP.
The resultant disturbance of water homeostasis causes the fluid accumulation seen in clinical disease. Neutrophils are the principal target of the oedema factor, which severely inhibits their function. Lethal toxin consists of lethal factor, a zinc metalloprotease, and protective antigen, which acts as the binding domain for oedema factor.
It causes the death of macrophages and other cells, including dendritic cells, neutrophils, and some epithelial and endothelial cells. In naturally occurring diseases, the local effects of the complex toxin include swelling and darkening of tissues due to oedema and necrosis. When septicemia occurs, increased vascular permeability and extensive haemorrhage lead to shock and rapid death.
Clinical infections:
Anthrax is the most important of these diseases. Bacillus licheniformis is an emerging pathogen as a cause of abortion in cattle and sheep. Bacillus cereus is important in human food poisoning and may cause an emetic or diarrhoeal syndrome. It is occasionally associated with cases of mastitis in cows.
Epidemiology:
Endospore formation is the most important factor in the persistence and spread of anthrax and is a response to nutrient depletion and other adverse environmental conditions. The endospores of B. anthracis can survive for decades in soil. Spores may become concentrated in some geographically defined regions where soil conditions favour spore survival.
Soils in such regions are alkaline, rich in calcium and nitrogen, and have a high moisture content. The increased survival of spores in alkaline, calcium-rich soils is because of the important role of calcium in the core of the spore.
Calcium, in combination with dipicolinic acid, forms a lattice that stabilizes the DNA and enzymes in the core and ensures spore survival. Leaching of calcium from the spore, which may occur in calcium-poor environments, impairs spore survival.
Outbreaks of anthrax disease in herbivores can occur when pastures are contaminated by spores originating from buried carcasses. Spores may be brought to the surface by flooding, excavation, subsidence, or the activity of earthworms.
Clinical signs and pathology:
The incubation period of anthrax ranges from hours to days. The clinical presentation and pathological changes vary with the species affected, the challenge dose, and the route of infection. In cattle and sheep, the disease is usually septicaemic and rapidly fatal.
Although most animals are found dead without premonitory signs, pyrexia with temperatures up to 42 °C (108 °F), depression, congested mucosae, and petechiae may be observed ante mortem. Animals that survive for more than a day may abort or display subcutaneous oedema and dysentery.
In cattle, post-mortem findings include rapid bloating, incomplete rigour mortis, widespread ecchymotic haemorrhages and oedema, dark, unclotted blood, and blood-stained fluid in body cavities. An extremely large, soft spleen is characteristic of the disease in cattle.
Splenomegaly and oedema are less prominent post – mortem features in affected sheep, which are reported to be more susceptible than cattle and succumb more rapidly. In dogs, which are rarely affected, the course of the disease and pathological changes resemble those observed in affected pigs.
Diagnosis
Carcasses of animals that have died from anthrax disease are bloated, putrefy rapidly, and do not exhibit rigour mortis. Dark, unclotted blood may issue from the mouth, nostrils, and anus. The carcasses of such animals should not be opened because this will facilitate sporulation, with the risk of long – term environmental contamination.
Culture and isolation are regarded as the gold standard for the diagnosis of disease. Blood agar and MacConkey agar are inoculated with the suspect specimens and incubated aerobically at 37 °C for 24 to 48 hours.
- Identification criteria for isolates:
- Colonial morphology
- Microscopic appearance in a Gram-stained
- smear
- Absence of growth on MacConkey agar
- PCR – based tests can be used to confirm the virulence of isolates by demonstrating the two virulence – associated plasmids, PXO1 and PXO2.
- Biochemical test profile.
This article is jointly authored by Muhammad Hamza, Ahmad Raza Fareed, Naeem Sarwar, Zill-e-Huma, Saif Ullah, Ayesha Arif, Palwasha Chandni, and Ambreen Noor from the University of Veterinary and Animal Sciences Lahore, subcampus Jhang.