Citing a telephone survey, the World Health Organization (WHO) observes that 20% Trusted Source of people aged 18–34 reported prolonged symptoms of kidney damage while having Covid-19
In December 2019, a coronavirus 2019 (COVID-19) disease outbreak occurred in Wuhan, Hubei Province, China, and rapidly spread to other areas worldwide. Around 10–15% Trusted Source of people who develop COVID-19 experience severe symptoms of kidney damage and approximately 5% become critically ill.
COVID common Signs and symptoms:
Most people who develop COVID-19 experience a mild or moderate illness that improves on its own. Some people who have had a mild or moderate illness go on to develop lasting symptoms that can be severe — even after they have recovered from the initial infection.
Long-Haulers:
People who have “long term COVID” effects with prolonged symptoms known as long haulers, may also have:
- extreme fatigue
- muscle weakness
- low-grade fever
- trouble concentrating
- lapses in memory
- mood changes
- trouble sleeping
- headaches
- a sensation of pins and needles
- diarrhea
- vomiting
- a loss of taste and smell
- a sore throat
- difficulties swallowing
- skin rashes
- shortness of breath
- chest pain
- heart palpitations
- the new onset of diabetes or high blood pressure
Relation of COVID and Kidney damage:
Kidney damage:
The kidneys are two bean-shaped organs below your rib cage. There’s one on each side of your spine. They do important jobs to keep you healthy. The kidneys are like filters that screen out toxins, extra water and waste products from the body. COVID-19 can cause tiny clots to form in the bloodstream, which can clog the smallest blood vessels in the kidney and impair its function, so that kidney damage occurs.
Researchers are finding evidence that COVID-19 can cause a host of symptoms and lead to a number of different complications, including ARDS and AKI.
Acute Kidney Infection (AKI)
In AKI disease kidney damage is severe enough and unable to properly filter the blood. This impairment causes waste products to build up in the blood, making it harder for the kidneys to work and maintain the body’s fluid balance. In severe or untreated cases, AKI can lead to organ failure, which can result in seizures, coma, and even death.
AKI is one of the most frequent and most severe organ complications in severe coronavirus disease 2019 (COVID-19). The SARS-CoV-2 virus has been detected in renal tissue. The increasing number of COVID-19 infected patients with renal involvement led to an evolving interest in the analysis of its pathophysiology, morphology and modes of virus detection in the kidney.
AKI was defined as an increase in serum creatinine by 0.3 mg/dl within 48 hours or a 50% increase in serum creatinine from baseline within 7 days according to the KDIGO criteria. The stage of AKI was determined using the peak serum creatinine level after AKI detection.
AKI Prevalence:
A recent review paper contradicts this finding, noting that an estimated 10% of people hospitalized for COVID-19 develop AKI. In a study from September 2020, 81% of patients admitted to the intensive care unit (ICU) for COVID-19 developed AKI.
In this large prospective cohort study conducted in a tertiary teaching hospital with 3 branches in Wuhan, China, we observed a high prevalence of kidney disease in hospitalized patients with COVID-19. 40% evidence of kidney disease are related with elevated serum creatinine and BUN values in over 13% of them. Strikingly, the presence of kidney disease was associated with greater in-hospital mortality.
COVID cycle in kidney damaging:
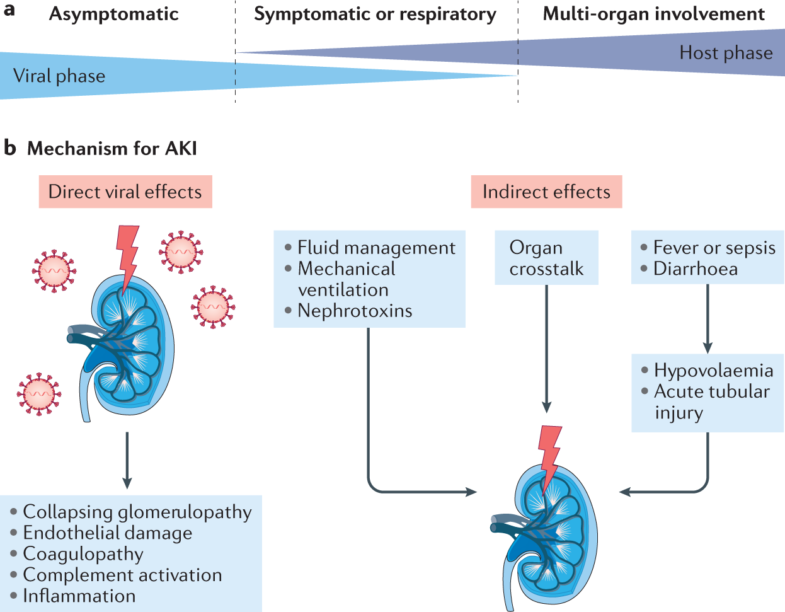
When SARS-CoV-2 virus attached to angiotensin converting enzyme 2 receptors. These receptors sit in the cellular membranes of cells lining the kidneys, lungs, gastrointestinal tract, heart, and arteries. They help moderate blood pressure by regulating levels of angiotensin, a protein that raises blood pressure by constricting blood vessels.
Some research suggests that SARS-CoV-2 may be more likely to target the kidneys as compared to the other parts of the body. It is because of ACE-2 expression is very high in the cells lining the proximal tubule. The proximal tubule is a major segment of the kidney responsible for the bulk of the reabsorption of water and nutrients from the blood.
Way of virus replication:
Once SARS-CoV-2 enters kidney cells, it begins to replicate using the cell’s machinery. Cells often sustain damage Trusted Source during this process. The immune system also sparks an inflammatory response once it recognizes the invading viral particles. This response can because of further damage to healthy tissue.
Racial disparities
Many studies found that race and ethnicity may influence the likelihood of developing AKI with COVID-19. 7% of people from Asia with COVID-19 experienced AKI. Several studies have found that Black people in the United States may be more likely to develop AKI with COVID-19.
In new research study, in New York that included 5,449 people hospitalized for COVID-19 found that Black people were 23% more than white people to develop AKI after adjusting for other health factors. In a study from October 2020, 48% of people who had AKI and were in the ICU with COVID-19 died in the hospital. 56% of people with kidney injury required dialysis.
Patient outcome
Based on the available research, it seems that AKI drastically increases the risk of severe COVID-19 and death. According to a recent meta-analysis, experiencing AKI with COVID-19 is associated with a 13-fold increase in mortality risk.