Groundbreaking research unveiled at this year’s ECCMID 2024 sheds new light on the dynamics of antimicrobial resistance (AMR) across Europe.
Groundbreaking research unveiled at this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2024) sheds new light on the dynamics of antimicrobial resistance (AMR) across Europe.
The study, conducted by a team led by Dr. Gwen Knight, Associate Professor at the London School of Hygiene and Tropical Medicine, and published in PLOS Medicine, underscores how levels of resistance to antimicrobials vary not only between countries but also according to age and sex.
To unravel the intricate web of AMR prevalence, researchers analyzed data from 29 European countries, encompassing over 6.8 million susceptibility results from bloodstream infections recorded between 2015 and 2019. The study delved into the relationship between age, sex, and AMR prevalence across different bacterial species and resistance phenotypes, utilizing advanced computer modeling techniques to discern patterns and trends.
The findings revealed a striking diversity in AMR prevalence across age groups and sexes, both within and between countries. Four main association forms emerged: a u-shaped pattern with a monotonic increase in resistance after infancy, a constant trend, an n-shaped curve with resistance peaking at intermediate ages, and a monotonic decline with age.
Surprisingly, while age showed substantial variation in association with resistance, the influence of sex was less pronounced, except in specific bacterial species like E. coli, K. pneumoniae, and Acinetobacter sp., where men were more susceptible to resistant infections at younger ages.
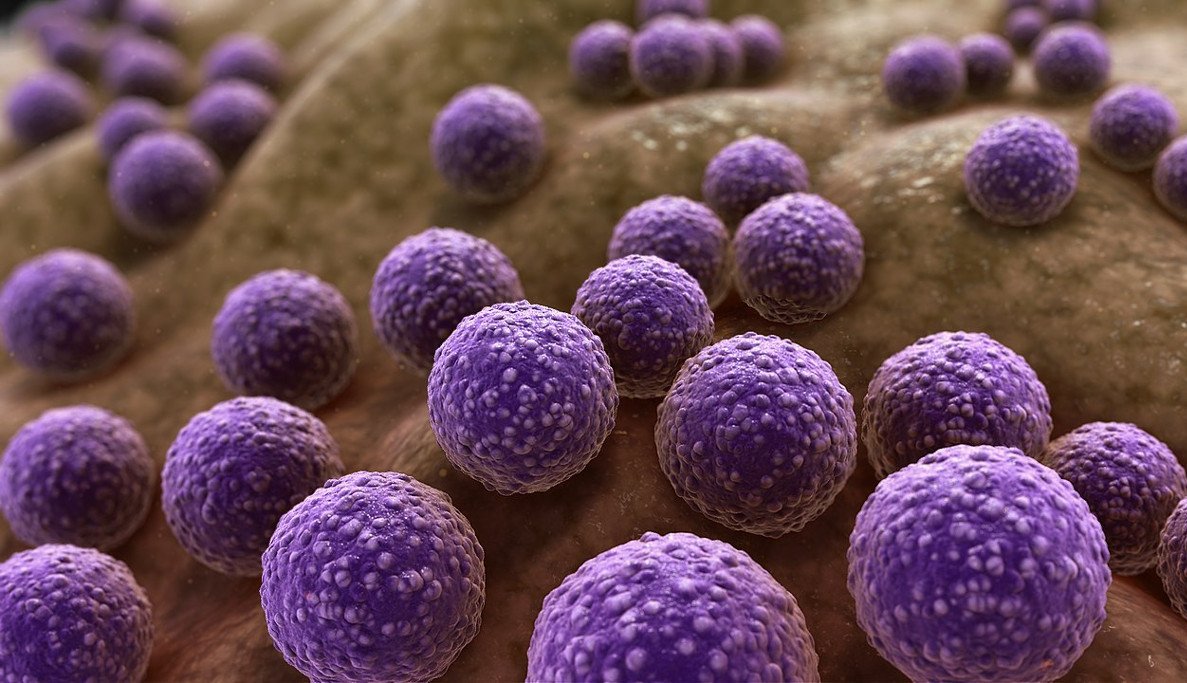
Moreover, the study highlighted variations in resistance trends at the European level, particularly within antibiotic families. For instance, methicillin-resistant Staphylococcus aureus (MRSA) exhibited a clear increase in resistance prevalence with age, while resistance to multiple antibiotics within Pseudomonas aeruginosa peaked around 30 years of age.
Conversely, trends for aminopenicillin resistance in Escherichia coli showed predominantly negative associations with age, indicating a decrease in resistance as individuals grew older.
Commenting on the unexpected findings, Dr. Gwen Knight remarked, “Most experts assume that resistance prevalence would increase with age due to cumulative antibiotic exposure effects and contact with healthcare settings, but it was not the case with all pathogens. I am also surprised by the fact that women, despite having more risk factors – such as childbirth and higher urinary tract infection incidence – and hence antibiotic exposures had a lower prevalence of resistant bloodstream infections.”
The study’s implications extend beyond mere epidemiological insights, raising crucial questions about intervention strategies and antibiotic usage guidelines. The authors stress the need for tailored interventions that account for the nuanced variations in AMR prevalence observed across different demographic groups.
“In light of these findings, there is a pressing need to reassess our approach to combating antimicrobial resistance,” emphasized Dr. Knight. “Understanding the complex interplay between age, sex, and resistance prevalence is essential for devising effective intervention strategies and optimizing antibiotic usage guidelines to mitigate the threat of AMR.”
The study underscores the importance of continued research and collaboration in the fight against antimicrobial resistance, urging policymakers, healthcare professionals, and researchers to work together to address this global health challenge.