CDC predicts a continued rise in JN.1 cases throughout the winter, marking it as a “variant of interest” according to the World Health Organization (WHO).
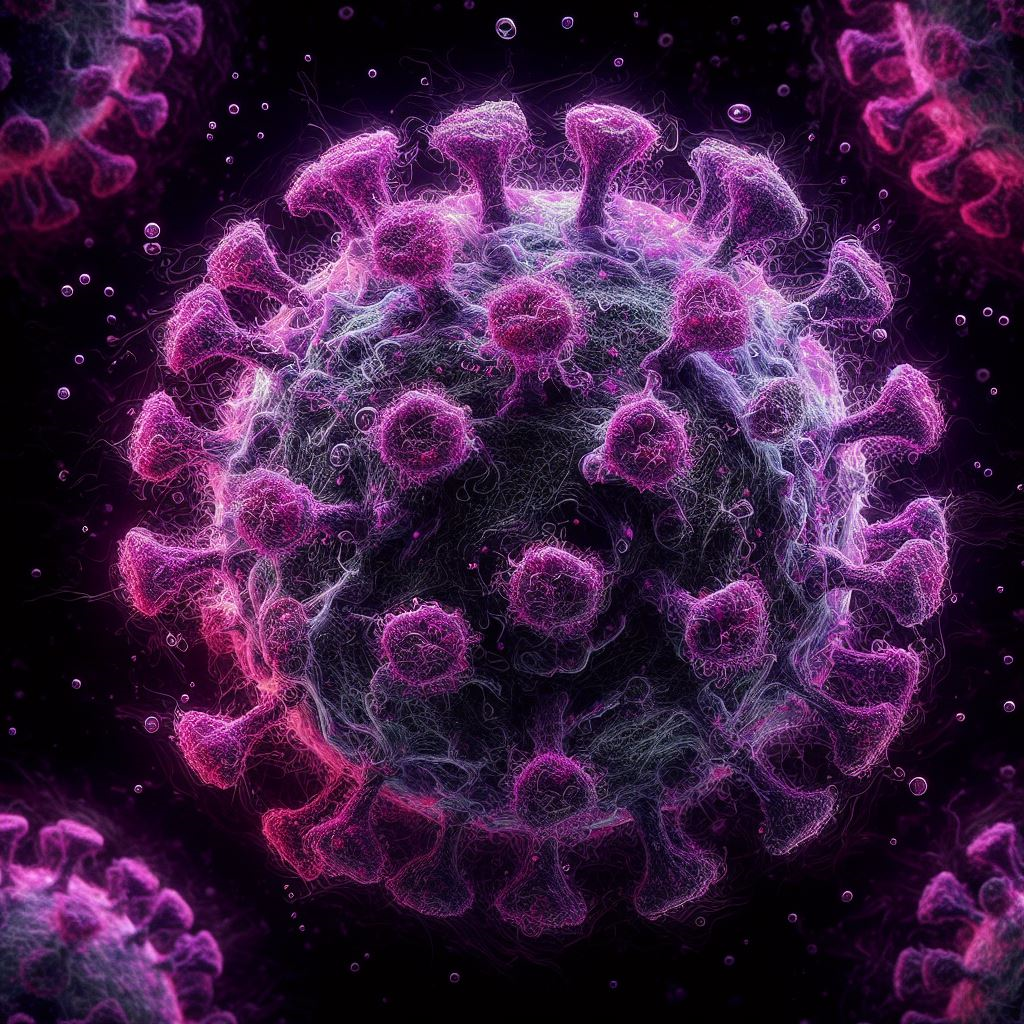
The JN.1 variant strain of the SARS-CoV-2 virus, which causes COVID-19, has quickly emerged as the most common strain in the US, accounting for more than 60% of cases as of early January, as cold weather drives people indoors and respiratory infections multiply. Concerns regarding the possibility of enhanced transmissibility or immune evasion have been raised by this spike in JN.1 infections.
The Centers for Disease Control and Prevention (CDC) predicts a continued rise in JN.1 cases throughout the winter, marking it as a “variant of interest” according to the World Health Organization (WHO). While there’s no evidence of heightened severity, the rapid spread suggests unique characteristics that warrant attention.
Dr. Heidi Zapata, an infectious diseases specialist at Yale Medicine, emphasizes the importance of acknowledging the ongoing evolution of the virus and the concurrent rise in overall COVID activity, including other variants like HV.1.
JN.1 emerged in the U.S. in September as a close relative of BA.2.86, informally known as “Pirola,” a lineage of the Omicron variant tracked by the CDC since August. Notably, JN.1 differs from BA.2.86 with a single mutation in its spike protein. Although the implications of this mutation are still under investigation, early research suggests potential enhanced immune evasion.
While evidence is still limited, JN.1 doesn’t appear to cause more severe cases or distinct symptoms compared to previous strains. The CDC emphasizes that COVID symptoms tend to be similar across variants, with individual immunity playing a crucial role in symptom severity. One striking aspect of JN.1 is its rapid evolution, growing from 3.5% to over 60% of cases within a few months.
Despite the recent uptick in COVID cases, it remains challenging to attribute this solely to JN.1 and other subvariants. The CDC had anticipated an increase in cases during the fall and winter based on historical patterns.
Amid concerns of a “tripledemic” with SARS-CoV-2, influenza, and RSV circulating simultaneously, preventive measures are crucial. Vaccines targeting all three illnesses are available for individuals aged 6 months and older, offering a layered defense against respiratory diseases. Additionally, specific RSV preventions are tailored for vulnerable populations.
Updated COVID vaccines introduced this fall aim to enhance protection against JN.1. COVID tests remain effective in detecting various strains, and antiviral treatments continue to be viable options. Protective measures, including strategic masking, hand-washing, improved ventilation, and monitoring local transmission levels, are key elements in reducing the risk of infection.
Dr. Zapata advises the public to stay informed, get updated vaccines, consider masking in specific situations, and undergo COVID testing if symptoms arise, as prompt detection allows for effective treatment.
As the winter unfolds, vigilance and a proactive approach to public health measures will play a pivotal role in mitigating the impact of evolving virus variants.