Intensifying therapy by adding carboplatin was found to be of benefit for one particular subgroup of pediatric high-risk medulloblastoma, findings from a phase III trial showed.
By Mike Bassett
Among children and young adults with high-risk medulloblastoma receiving craniospinal radiotherapy plus vincristine, the 5-year event-free survival (EFS) rate was 66.4% for those that treated with carboplatin, as compared to 59.2% for those who did not, a non-significant advantage (P=0.11), reported Sarah Leary, MD, of the Cancer and Blood Disorders Center at Seattle Children’s, and colleagues.
But in patients with high-risk group 3 medulloblastoma, adding carboplatin improved the EFS rate from 53.7% to 73.2% at 5 years (P=0.047). The 5-year overall survival (OS) rate for this population was 63.7% without carboplatin and 82.8% with it (P=0.06), according to the findings in JAMA Oncology.
However, this intensified therapy came with increased toxicity, particularly hematologic effects such as thrombocytopenia and febrile neutropenia, as well as neurocognitive effects.
“It is therefore appropriate to avoid therapy intensification in groups of patients who would not be expected to benefit, specifically in those with WNT [signaling pathway activated], SHH [signaling pathway activated], and group 4 medulloblastoma,” the authors wrote.
“Based on the results of this prospective randomized clinical trial, concurrent carboplatin treatment during radiotherapy is recommended for pediatric patients with high-risk group 3 medulloblastoma and not recommended in other populations,” Leary and colleagues concluded, adding that “a rapid, comprehensive integrated molecular diagnosis is necessary for medulloblastoma risk stratification.”
The added toxicity of therapy intensification underscores the importance of correctly identifying patients who will benefit from the therapy, in order to avoid unnecessary suffering, said Allison Martin, MD, of Albert Einstein College of Medicine in New York City, and Sadhana Jackson, MD, of the National Cancer Institute in Bethesda, Maryland, in an accompanying commentary.
The study “provides us with glimmers of hope for the survival of children with high-risk group 3 medulloblastoma and that the treatment paradigm for all patients with high-risk disease can be improved through incorporation of detailed molecular analyses,” Martin and Jackson wrote.
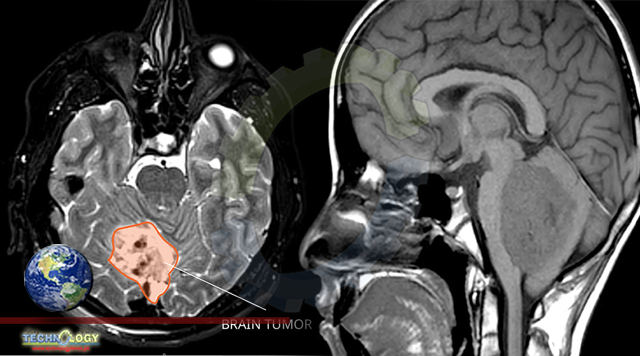
Medulloblastoma is the most common type of cancerous brain tumor in children (median age 8 years), but most patients can be cured with a combination of treatments, including neurosurgical resection, craniospinal radiation, and combination chemotherapy. However, Leary and colleagues pointed out that there are few therapeutic options in the event of relapse. “Evaluation of therapeutic interventions to prevent relapse is warranted,” they noted.
This multi-institutional Children’s Oncology Group study evaluated therapy intensification with carboplatin as a radiosensitizer and isotretinoin as a proapoptotic agent in patients ages 3 to 21 years with newly diagnosed high-risk medulloblastoma (metastatic disease, diffuse anaplastic histologic characteristics, or incomplete surgical resection defined as greater than 1.5 cm2 residual tumor) from March 2007 to September 2018.
Patients were randomized to receive 36-Gy craniospinal radiation therapy and weekly vincristine with or without daily carboplatin followed by 6 cycles of maintenance chemotherapy with cisplatin, cyclophosphamide, and vincristine with or without 12 cycles of isotretinoin during and following maintenance.
This study was initially powered to evaluate medulloblastoma as a single disease. It was later amended, however, to include a molecular subgroup analysis according to World Health Organization consensus molecular subgroups of medulloblastoma (WNT, SHH, group 3, and group 4). The primary endpoint was EFS.
The study included 294 patients, 261 (median age 8.6 years, 70% males) of whom were evaluable after central radiologic and pathologic review. Of these patients, 189 (72%) had metastatic disease, 58 (22%) had diffuse anaplasia, and 14 (5%) had greater than 1.5-cm2 residual disease.
For all patients, the 5-year EFS and OS rates were 62.9% (95% CI 55.6-70.2) and 73.4% (95% CI 66.7-80.1), respectively.
Randomization of isotretinoin was discontinued when it was determined that it would not lead to significant differences in EFS.
Originally published at Medpage today