The researchers gives global study and suggest the need for psychological support for COVID-19 survivors is still greater than for the typical ICU patient who may suffer post-traumatic stress disorder (PTSD), among other issues.
After COVID-19, Discharge Doesn’t Always Mean Recovery
An earlier study reports on 143 Italian patients at 60 days from the end of hospitalization. Follow-up showed that at least one symptom was still present in 87% of the patients at this time point; over half had 3 or more symptoms.
The commonly reported symptoms include fatigue in more than half, joint pain in over a quarter, and chest pain in more than a fifth of these patients. A little less than half said COVID-19 had impaired their quality of life.
It is notable that some patients with mild COVID-19 also did not seem able to shake off the illness. Again, neurological complications are known to happen with COVID-19, including brain involvement as in encephalitis or encephalopathy, and psychiatric diagnoses, in the acute phase, but their long-term outcome is unknown.
Long-Term Follow-Up
The current paper lays out the details of a longitudinal study that aims to follow up COVID-19 patients, including any pre-existing chronic illnesses as well as the medical care they received during their illness. A significant minority of convalescents appears to have prolonged disease sequelae.
Some, such as carbon monoxide accumulation due to impaired lung function, and PTSD, as well as other mood disorders, have been documented following the earlier outbreaks of SARS and MERS, in 30% to 40%. In the current pandemic, the accompanying widespread loss of earning capacity and social interactions are additional stress factors operating on a large scale.
In particular, they say, they want to find out how these are linked to chronic conditions. The possibility of sequelae arises from the fact that severe COVID-19 illness leads to acute respiratory distress, severe lung damage, and multiorgan failure in some cases, including heart, liver, and kidney injury.
In many cases, the patient also has systemic inflammation and often circulatory shock. The high level of inflammation and acute hypoxia are known risk factors for cognitive decline.
The researchers aimed to uncover the global study patterns of mental and physical sequelae to COVID-19, and the risk factors for such consequences, as well as the temporal immune responses, the presence of protective immunity, and the need for rehabilitation in this patient group. The expected outcomes include better management and public health strategies.
The Protocols and Cases
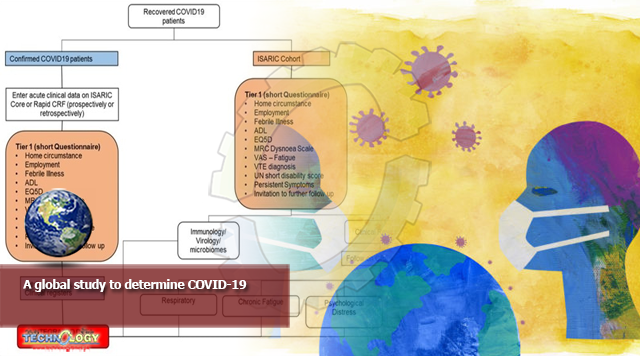
The protocol for the study was developed by the International Severe Acute Respiratory and Emerging Infection Consortium (ISARIC) COVID-19 follow up working group. The researchers aim to cover all categories of discharged COVID-19 patients except children. The open-access study is designed to be an international multicenter prospective study with an observational protocol.
All participants will have a positive diagnosis of COVID-19, being aged at least 16 years, and at least 28 days from discharge.
The case report form (CRF) is based on the Clinical Characterization Protocol (CCP), a standardized reporting format for rapid and reliable collection of data and bio-samples in a uniform manner worldwide, that can be adapted for acute or follow-up reporting for any severe acute infection which is vital for public health.
Along with the CRF, samples of respiratory secretions, blood, urine, and stool will be collected from some patients. The researchers will then analyze the data for variations in the outcomes across age groups, socioeconomic groups, and other demographic variables, as well as in the presence of several chronic illnesses, exposures to, and the complications that occurred in the acute phase of COVID-19, or their hospital stay. This is expected to help both public health bodies and researchers progress their work.
The first tier of the study is for patient follow-up at 28 days, and then at intervals of 3-6 months, to pick out those patients who have certain specific symptoms for more extended evaluation.
The second tier aims at a detailed follow-up in a clinic to describe the physical sequelae. Other outcomes are finding out the estimated proportion of patients with such consequences and the risk factors, the social and mental sequelae, and how many people die of the illness directly or indirectly after being discharged.
Specific post-COVID-19-mortality causes that will be evaluated include deep vein thrombosis, pulmonary embolism, recent fevers, and new symptoms of a non-transient nature. Dyspnea, disability, lifestyle, and job-related factors will also be included in the analysis.
Conclusions
The final data and results will be posted both in open-access publications and on the ISARIC website for the benefit of the medical and broader scientific community to take appropriate action.
The researchers says by global study, “The outcomes of this study will inform strategies to prevent long term consequences; inform clinical management, direct rehabilitation, and inform public health management to reduce overall morbidity and improve outcomes of COVID-19.”
Originally published at News medical