Leishmaniasis is a term used to describe a number of closely related diseases caused by about 30 distinct species, subspecies and strains of Leishmania parasites.
 In around the World, there are about 1–2 million cases a year, with about 12 million people currently infected in 88 countries. In both the Old and New Worlds, sand flies are the vectors of leishmaniasis, Leishmania species in Pakistan are; L.Major: (In Balochistan, sindh and Punjab) & L.Tropics: (In Khyber pakhtunkhwa and Fata).
In around the World, there are about 1–2 million cases a year, with about 12 million people currently infected in 88 countries. In both the Old and New Worlds, sand flies are the vectors of leishmaniasis, Leishmania species in Pakistan are; L.Major: (In Balochistan, sindh and Punjab) & L.Tropics: (In Khyber pakhtunkhwa and Fata).
The vectors live in damp dark places and weak flyers, vectors can fly only 150m from breeding site. The viruses are responsible for sand fly fever, and the bacterium responsible for Bartonella bacilliformis, causing bartonellosis.
The epidemiology of leishmaniasis is complex, involving not only different parasite species but different strains of parasites and different reservoir hosts. Basically amastigote parasites ingested by female sand flies with a blood-meal multiply in the gut and develop into promastigotes, which are elongate, have a flagellum and attach to the mid-gut or hind-gut wall and multiply rapidly.
Culturing of promastigotes
The promastigotes of leishmania were grown in a medium containing;
- Rpm 199 medium
- With 10% fetal calf serum (FCS)
- HEPES buffer
- Streptomycin
- Penicillin
Here some parasites become metacyclic forms. Four to 25 days after the sand fly has taken an infective blood-meal the metacyclic forms are found in the mouthparts, and are introduced into a new host during feeding. Most types of leishmaniasis are zoonoses. The degree of involvement of humans varies greatly from area to area.
The epidemiology is largely Medical importance determined by the species of sand flies, their ecology and behaviour, the availability of a wide range of non-human hosts, and also by the species and strains of Leishmania parasites.
In some areas, for example, sand flies will transmit infections almost entirely among wild or domesticated animals, with little or no human involvement, whereas elsewhere animals may be important reservoir hosts of infection for humans. The epidemiology of the leishmaniasis is complex.
The three main clinical forms are cutaneous, mucocutaneous and visceral leishmaniasis.A fourth, less common form is diffuse cutaneous leishmaniasis, while post-kala-azar dermal leishmaniasis is caused by Leishmania donovani donovani following cure of the initial visceral form.
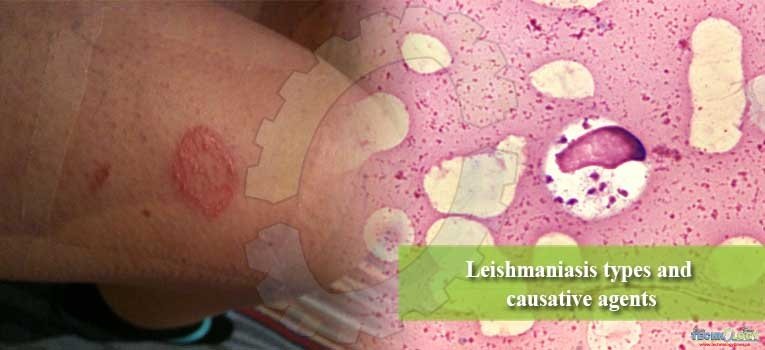
1.Cutaneous leishmaniasis (CL)
In the Old World, CL is also known as oriental sore. It occurs mainly in arid areas of the Middle East to northwestern India and central Asia, in North Africa and various areas in East, West and southern Africa.
The principal parasites are Leishmania major, transmitted mainly by Phlebotomus papatasi, and Le. tropica, transmitted by P. sergenti. Leishmania major is usually zoonotic and in most of its range gerbils (e.g. Rhombomys opimus) are the reservoir hosts; Le. tropica occurs in densely populated areas and humans appear to be the main reservoir hosts.
In the New World, CL is found mainly in forests from Mexico to northern Argentina, and is caused by Leishmania braziliensis, Le. amazonensis and Le. mexicana. Rodents and dogs appear to be reservoir hosts. Lutzomyia wellcomei and L. flaviscutellata are its vectors.
Clinical features of cutaneous leishmaniasis:
- Larger ulcer of 5-10mm or moist type lesions having reddish raised edge.
- Self-healing within 3-9 month in case of leishmaniasis infection (Neva& Brown,1994).
- tropica causes dry-type lesions 25-70mm.
- Lesions heal within 8-15 months having a scar.
2. Mucocutaneous leishmaniasis (ML)
It is mainly caused by Leishmania braziliensis. It is a severely disfiguring disease found from Mexico to Argentina. Dogs may be reservoir hosts. Lutzomyia wellcomei is an important vector.
3. Diffuse cutaneous leishmaniasis (DCL)
A form that causes widespread cutaneous nodules or macules over the body. It is confined to Venezuela and the Dominican Republic and the highlands of Ethiopia and Kenya.
In South America the parasite is Le. amazonensis, transmitted by Lutzomyia flaviscutellata, and spiny rats (Proechimys species) are reservoir hosts.
4.Visceral leishmaniasis (VL)
Often referred to askala-azar. It is caused by Leishmania donovani donovani in most areas of its distribution, such as India, Bangladesh, Sudan, East Africa and Ethiopia. Among the vectors are Phlebotomus argentipes and P. orientalis. Rodents, wild cats and genets (Genetta genetta) may be reservoir hosts.
Dogs and foxes (Vulpes vulpes) are reservoir hosts. Visceral leishmaniasis also occurs sporadically in Central and South America, where the parasite is Le. donovani infantum, transmitted by species in the Lutzomyia longipalpis complex.
Over 60% of visceral leishmaniasis occurs in India, Bangladesh and Nepal, and an estimated 150 million people are at risk. In 2005 these countries signed an agreement to eliminate VL by 2015, mainly based on integrated vector control.
Note: In both the Old and New Worlds, sand flies are the vectors of leishmaniasis and viruses responsible for sand fly fever, and the bacterium responsible for Bartonella bacilliformis, causing bartonellosis.
Sand fly fever
Sand flies transmit the seven viral serotypes responsible for sandfly fevers, also called papataci fever (sometimes spelt papatasi or pappataci fever), three-day fever or Phlebotomus fevers.
The classical form of the disease is found in the Mediterranean region, but it also extends up the Nile into Egypt, and from the Middle East to northern India, Pakistan, Afghanistan and China. The most important vectors in the Old World are P. papatasi and P. perniciosis.
Female sand flies become infective 7–10 days after taking a blood-meal. Infected females lay eggs containing the virus, and these eventually give rise to infected adults. This is an example of transovarial transmission, a phenomenon that is more common in the transmission of various tick-borne diseases.
There are possibly mammalian reservoir hosts, but in many areas it is likely that humans are the main reservoir of infection. Sand fly fever virus is recognized as a potential bioterrorism agent.
Bartonellosis
Bartonellosis, sometimes called Oroya fever or Carrión’s disease, is encountered in arid mountainous areas of the Andes, mainly in Peru, but also in Ecuador and Colombia.
It is caused by the bacterium Bartonella bacilliformis and is transmitted in Peru by Lutzomyia verrucarum and L. peruensis, and by L. colombiana in Colombia, but there are probably other vectors. It is transmitted by the contamination of mouthparts. Apart from humans, there are no other vertebrate reservoir hosts.
Control
Characterization of chemicals
- Preliminary phytochemicals screening by using different phytochemical tests.
- UV-Vis spectroscopy.
- Fourier transform infrared spectroscopy.
- Gas chromatograph coupied mass spectroscopy (GC-MS).
- Although phlebotomine sand flies are very susceptible to insecticides, until recently there have been few organized attempts to control them. However, in most areas where house-spraying has been used to control Anopheles vectors there have been large reductions in sand fly populations followed by interruption of leishmaniasis transmission. When houses in Kabul, Afghanistan, and in the Peruvian Andes were sprayed with the pyrethroid lambda-cyhalothrin, cutaneous leishmaniasis was reduced by 60% and 54% respectively.
- In areas where sand flies rest indoors, cattle sheds and chicken houses should also be sprayed. Obviously where sand flies bite and rest out of doors house-spraying will have little effect. However, if the outdoor resting sites are known (e.g. animal shelters, stone walls, tree trunks, termite hills), they can be sprayed with residual insecticides. Insecticidal fogging of outdoor resting sites may also give some, but temporary, control of vectors.
- Personal protection can be achieved by applying efficient insect repellents such as DEET, piperidene-based ones and neem oil.
- Insecticide-impregnated bed-nets such as the long-lasting Olyset nets will give protection from sand fly biting. For example, in Afghanistan and Syria insecticide treated polyester bed-nets gave good protection against Phlebotomus sergenti, an important vector of cutaneous leishmaniasis (Le. tropica).
- Control of sand fly larvae remains impossible, because the breeding sites of most species are unknown.Because most leishmaniasis transmission involves reservoir hosts, such as rodents and dogs, attempts have been made to destroy them.
Conclusion
- Cutaneous leishmaniasis is prevalent in district Dir, Pakistan.
- It effects both the gender of all ages and can be prevalent throughout the year.
- Anti-leishmanial activity of P.camescens was much higher than the control drug Amphotericin B.
Recommendations
- The anti-leishmanial assay was directed on one L.tropica, the same work must be carried out on large variety of leishmania strains in order to have clear idea of the spectrum of anti-leishmanial activity of these slected plants extract.
- The in-vitro antileishmanial activity of the extracts were done, so further detailed in-vitro studies are recommended on rodents.
- More investigations can done for obtaining a novel drug like triterpenoids that could potentially be less toxic and more cost-effective against the leishmania parasite.
AUTHORS: Arzlan Abbas, Saddam Hussain and Muhammad Ayoub
CORRESPONDING AUTHOR: Arzlan Abbas